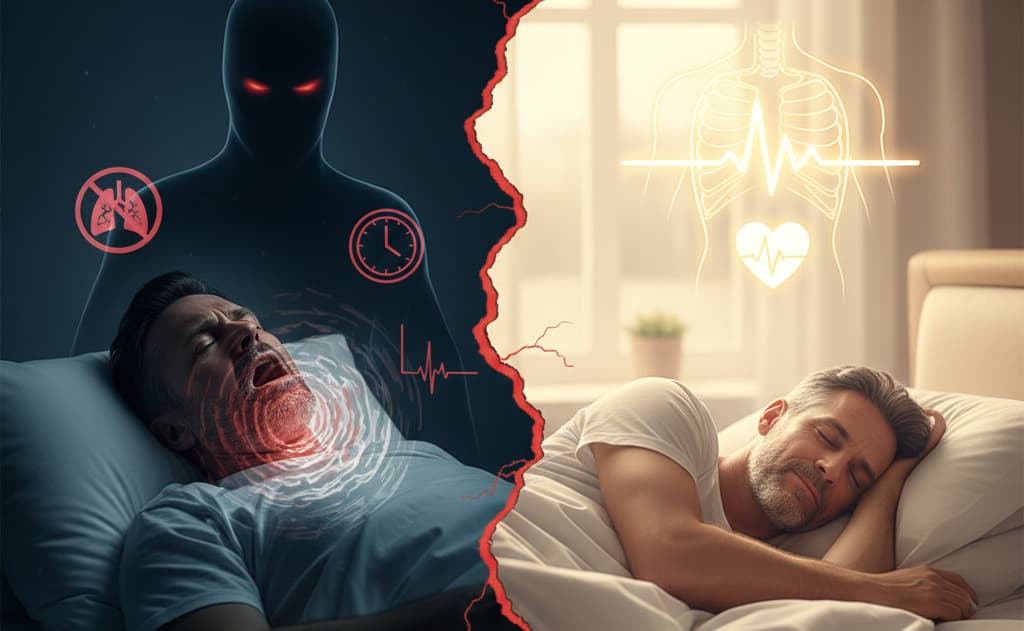
Snoring, which many people might consider a minor annoyance, is often a typical symptom of Obstructive Sleep Apnea (OSA). OSA is a common sleep disorder where individuals repeatedly experience partial or complete blockage of the upper airway during sleep, leading to breathing pauses and low blood oxygen levels. This not only severely affects sleep quality but can also trigger various complications like hypertension, heart disease, and diabetes.
What is Obstructive Sleep Apnea (OSA)?
Before understanding sleep apnea machines, let’s briefly introduce OSA. When a person falls asleep, the muscles in the throat relax. If they relax too much or if there’s excess tissue (like tonsils, soft palate, or tongue base), the airway can collapse or narrow, preventing air from passing smoothly.
Common Symptoms of OSA
- Habitual, loud snoring, possibly with sudden interruptions
- Choking, gasping, or breathing pauses during sleep (often noticed by a partner)
- Increased nighttime urination
- Morning dry mouth or headache
- Daytime sleepiness, fatigue, and difficulty concentrating
- Memory decline and mood changes (e.g., irritability, anxiety)
How Do Sleep Apnea Machines Work?
Sleep apnea machines deliver a continuous stream of air at a specific pressure into the patient’s airway, creating an “air splint” that prevents the upper airway from collapsing during sleep, thus keeping it open.
CPAP (Continuous Positive Airway Pressure) Machine
This is the most common type. It delivers a constant airflow pressure throughout the respiratory cycle. CPAP machines are effective for most patients with OSA and are typically the first-line treatment.
APAP (Automatic Positive Airway Pressure) Machine
Can automatically adjust the output pressure based on changes in the patient’s airway resistance during sleep. For example, it lowers pressure when the airway is open and increases it when a collapse is imminent, offering relatively higher comfort.
BiPAP (Bilevel Positive Airway Pressure) Machine
Provides two different pressure levels – higher during inhalation and lower during exhalation. Mainly used for patients who cannot tolerate CPAP pressure or have coexisting respiratory conditions (like COPD).
Who is Suitable for Using a Sleep Apnea Machine?
Sleep apnea machines are primarily suitable for:
Suitable Candidates
- Patients diagnosed with moderate to severe Obstructive Sleep Apnea (OSA) through polysomnography
- Mild OSA patients who experience significant daytime sleepiness, hypertension, cardiovascular diseases, or other complications
- Some patients with Central Sleep Apnea (CSA) or mixed sleep apnea, who require specific types of machines under a doctor’s guidance
Key Takeaways
Sleep apnea machines, particularly CPAP devices, are currently one of the most effective treatments for moderate to severe OSA. Understanding the working principles, suitable users, selection criteria, and usage precautions is crucial for successful treatment.
Remember: The decision to use a sleep apnea machine should always be made under professional medical guidance. If you suspect you have sleep apnea, consult with a healthcare provider for proper diagnosis and treatment recommendations.
Self test insomnia: comprehensive assessment tools and when to seek help

Recognizing and understanding your sleep patterns is the first step toward addressing insomnia. Self-assessment tools can help you identify sleep problems, track patterns, and determine when professional help might be needed. This comprehensive guide provides validated assessment tools and practical strategies for evaluating your sleep health.
Understanding Insomnia: Types and Symptoms
What is Insomnia?
Clinical definition:
- Difficulty falling asleep (sleep onset insomnia)
- Difficulty staying asleep (sleep maintenance insomnia)
- Early morning awakening with inability to return to sleep
- Non-restorative sleep despite adequate sleep opportunity
- Daytime impairment as a result of sleep difficulties
Duration criteria:
- Acute insomnia: Less than 3 months, often triggered by stress or life changes
- Chronic insomnia: 3 or more nights per week for 3 months or longer
- Episodic insomnia: Recurring periods of sleep difficulties
Common Insomnia Symptoms
Nighttime symptoms:
- Taking more than 30 minutes to fall asleep
- Waking up frequently during the night
- Staying awake for long periods during the night
- Waking up too early and being unable to fall back asleep
- Feeling unrefreshed upon waking
Daytime symptoms:
- Fatigue or low energy
- Difficulty concentrating or remembering
- Mood disturbances (irritability, anxiety, depression)
- Decreased performance at work or school
- Increased errors or accidents
- Tension headaches
- Gastrointestinal symptoms
- Ongoing worries about sleep
Insomnia Severity Index (ISI) Self-Assessment
The Insomnia Severity Index
The ISI is a validated 7-item questionnaire designed to assess the nature, severity, and impact of insomnia. Rate each item from 0-4 based on your experience over the past two weeks:
Question 1: Difficulty falling asleep
- 0 = None
- 1 = Mild
- 2 = Moderate
- 3 = Severe
- 4 = Very severe
Question 2: Difficulty staying asleep
- 0 = None
- 1 = Mild
- 2 = Moderate
- 3 = Severe
- 4 = Very severe
Question 3: Problems waking up too early
- 0 = None
- 1 = Mild
- 2 = Moderate
- 3 = Severe
- 4 = Very severe
Question 4: How satisfied/dissatisfied are you with your current sleep pattern?
- 0 = Very satisfied
- 1 = Satisfied
- 2 = Moderately satisfied
- 3 = Dissatisfied
- 4 = Very dissatisfied
Question 5: How noticeable to others do you think your sleep problem is in terms of impairing the quality of your life?
- 0 = Not at all noticeable
- 1 = A little
- 2 = Somewhat
- 3 = Much
- 4 = Very much noticeable
Question 6: How worried/distressed are you about your current sleep problem?
- 0 = Not at all worried
- 1 = A little
- 2 = Somewhat
- 3 = Much
- 4 = Very much worried
Question 7: To what extent do you consider your sleep problem to interfere with your daily functioning?
- 0 = Not at all interfering
- 1 = A little
- 2 = Somewhat
- 3 = Much
- 4 = Very much interfering
ISI Scoring and Interpretation
Total your scores (0-28 points):
- 0-7 points: No clinically significant insomnia
- 8-14 points: Subthreshold insomnia (mild)
- 15-21 points: Clinical insomnia (moderate severity)
- 22-28 points: Clinical insomnia (severe)
What your score means:
- 0-7: Your sleep appears to be within normal limits
- 8-14: You may have mild sleep difficulties that could benefit from sleep hygiene improvements
- 15-21: You likely have moderate insomnia that may require professional evaluation
- 22-28: You have severe insomnia that definitely warrants professional treatment
Sleep Diary: Tracking Your Patterns
How to Keep a Sleep Diary
Daily tracking items:
- Bedtime: What time you got into bed
- Sleep onset time: Estimated time you fell asleep
- Sleep onset latency: How long it took to fall asleep
- Number of awakenings: How many times you woke up
- Wake after sleep onset: Total time awake during the night
- Final wake time: When you woke up for the day
- Get-up time: When you got out of bed
- Total sleep time: Estimated actual sleep duration
- Sleep quality rating: Rate 1-10 (1=very poor, 10=excellent)
Additional factors to track:
- Caffeine intake (amount and timing)
- Alcohol consumption
- Exercise (type, duration, timing)
- Naps (duration and timing)
- Medications taken
- Stress level (1-10 scale)
- Mood upon waking
- Daytime sleepiness level
Sleep Efficiency Calculation
Sleep efficiency formula:
- Sleep Efficiency = (Total Sleep Time ÷ Time in Bed) × 100
- Time in Bed = Get-up time – Bedtime
- Total Sleep Time = Time in Bed – Sleep Onset Latency – Wake After Sleep Onset
Sleep efficiency interpretation:
- 85% or higher: Normal sleep efficiency
- 80-84%: Mild sleep efficiency problems
- 75-79%: Moderate sleep efficiency problems
- Below 75%: Significant sleep efficiency problems
Example calculation:
- Bedtime: 10:30 PM
- Get-up time: 6:30 AM (8 hours in bed)
- Sleep onset latency: 45 minutes
- Wake after sleep onset: 30 minutes
- Total sleep time: 8 hours – 45 min – 30 min = 6 hours 45 minutes
- Sleep efficiency: (6.75 ÷ 8) × 100 = 84.4%
Digital Sleep Tracking Tools
Smartphone apps:
- Sleep Cycle: Uses sound analysis to track sleep phases
- Pillow: Automatic sleep tracking with heart rate monitoring
- Sleep Score: Comprehensive sleep tracking and coaching
- AutoSleep (Apple Watch): Automatic sleep detection
Wearable devices:
- Fitbit devices: Track sleep stages, duration, and quality
- Apple Watch: Sleep tracking with bedtime reminders
- Oura Ring: Detailed sleep analysis and recovery metrics
- Garmin watches: Sleep monitoring with stress tracking
Limitations to consider:
- Consumer devices may not be as accurate as clinical tools
- Movement-based tracking can misinterpret restless wakefulness as sleep
- Should supplement, not replace, subjective sleep diary data
- May increase sleep anxiety in some individuals
Additional Self-Assessment Tools
Epworth Sleepiness Scale
Rate your likelihood of dozing off in these situations (0-3 scale):
0 = Would never doze, 1 = Slight chance, 2 = Moderate chance, 3 = High chance
- Sitting and reading
- Watching TV
- Sitting inactive in a public place
- As a passenger in a car for an hour without a break
- Lying down to rest in the afternoon
- Sitting and talking to someone
- Sitting quietly after lunch without alcohol
- In a car, while stopped for a few minutes in traffic
Scoring:
- 0-5: Lower normal daytime sleepiness
- 6-10: Higher normal daytime sleepiness
- 11-12: Mild excessive daytime sleepiness
- 13-15: Moderate excessive daytime sleepiness
- 16-24: Severe excessive daytime sleepiness
Sleep Hygiene Assessment
Rate how often you do the following (Never/Sometimes/Often/Always):
- Go to bed at the same time each night
- Wake up at the same time each morning
- Use your bedroom only for sleep and intimacy
- Keep your bedroom cool, dark, and quiet
- Avoid caffeine 6 hours before bedtime
- Avoid alcohol 3 hours before bedtime
- Avoid large meals 2-3 hours before bedtime
- Exercise regularly, but not close to bedtime
- Have a relaxing bedtime routine
- Avoid screens 1 hour before bedtime
- Get natural light exposure during the day
- Limit daytime naps to 20-30 minutes
Assessment:
- Mostly “Always” and “Often”: Good sleep hygiene
- Mix of responses: Room for improvement in sleep habits
- Mostly “Sometimes” and “Never”: Poor sleep hygiene requiring attention
Pre-Sleep Arousal Scale
Rate how intensely you experience these symptoms as you attempt to fall asleep:
Cognitive arousal symptoms:
- Racing thoughts
- Worry about falling asleep
- Review or ponder events of the day
- Worry about problems other than sleep
- Being mentally alert, active
- Unable to shut down thoughts
- Thoughts keep running through your head
- Being distracted by sounds, noise in the environment
Somatic arousal symptoms:
- Heart racing, pounding, or beating irregularly
- Shortness of breath or labored breathing
- A jittery, nervous feeling in your body
- Muscle tension or tightness
- Cold feeling in hands, feet, or your body in general
- Having stomach upset
- Perspiration in palms of your hands or other parts of your body
Rating scale: 1 = Not at all, 2 = Slightly, 3 = Moderately, 4 = A lot, 5 = Extremely
When to Seek Professional Help
Red Flags Requiring Immediate Attention
Serious symptoms:
- Loud snoring with gasping or choking sounds
- Witnessed breathing pauses during sleep
- Excessive daytime sleepiness affecting safety (driving, work)
- Sudden onset of severe insomnia
- Sleep problems accompanied by chest pain or shortness of breath
- Sleepwalking or other unusual sleep behaviors
- Violent or aggressive behavior during sleep
Mental health concerns:
- Thoughts of self-harm or suicide
- Severe depression or anxiety
- Hallucinations or delusions
- Significant mood changes affecting daily life
When to Consult a Healthcare Provider
Duration criteria:
- Sleep problems persisting for more than 2-3 weeks
- Chronic insomnia (3+ nights per week for 3+ months)
- Sleep issues significantly impacting daily functioning
- Multiple failed attempts at self-help strategies
Severity indicators:
- ISI score of 15 or higher
- Epworth Sleepiness Scale score of 11 or higher
- Sleep efficiency consistently below 80%
- Taking more than 45 minutes to fall asleep regularly
- Waking up 3+ times per night regularly
Impact on daily life:
- Difficulty concentrating at work or school
- Increased errors or accidents
- Relationship problems due to irritability
- Physical symptoms (headaches, GI issues)
- Reliance on caffeine or other stimulants
Types of Sleep Specialists
Primary care physician:
- First point of contact for sleep concerns
- Can rule out medical causes of insomnia
- May prescribe initial treatments
- Can refer to specialists when needed
Sleep medicine specialist:
- Board-certified in sleep medicine
- Specializes in all types of sleep disorders
- Can order sleep studies if needed
- Provides comprehensive sleep disorder treatment
Behavioral sleep medicine specialist:
- Psychologist specializing in sleep disorders
- Provides cognitive behavioral therapy for insomnia (CBT-I)
- Addresses psychological factors affecting sleep
- Non-medication treatment approaches
Psychiatrist:
- When sleep problems are related to mental health conditions
- Can prescribe medications for sleep and mood disorders
- Addresses underlying psychiatric conditions
- Comprehensive mental health evaluation
Preparing for Your Healthcare Visit
Information to Gather
Sleep history:
- Completed sleep diary (2-4 weeks minimum)
- Self-assessment questionnaire results
- Timeline of when sleep problems began
- Previous treatments tried and their effectiveness
- Family history of sleep disorders
Medical information:
- Current medications and supplements
- Medical conditions and recent changes
- Recent life stressors or changes
- Substance use (caffeine, alcohol, tobacco)
- Work schedule and shift patterns
Symptom details:
- Specific sleep complaints and their frequency
- Daytime symptoms and their impact
- What makes symptoms better or worse
- Sleep environment description
- Bed partner observations
Questions to Ask Your Healthcare Provider
Diagnostic questions:
- What type of sleep disorder do I likely have?
- What tests or evaluations do you recommend?
- Could my medications be affecting my sleep?
- Are there underlying medical conditions to consider?
Treatment questions:
- What treatment options are available?
- What are the benefits and risks of each option?
- How long before I see improvement?
- What can I do at home to help?
- When should I follow up?
Lifestyle questions:
- Are there activities I should avoid?
- How will this affect my work or daily activities?
- What warning signs should I watch for?
- Are there resources or support groups you recommend?
Taking Control of Your Sleep Health
Self-assessment is a valuable first step in understanding and addressing sleep problems. By using validated tools, keeping detailed sleep records, and knowing when to seek professional help, you can take an active role in improving your sleep health.
Remember: While self-assessment tools are helpful for understanding your sleep patterns, they don’t replace professional medical evaluation. If your sleep problems are significantly impacting your life, don’t hesitate to seek help from a qualified healthcare provider.
The Hidden Dangers of Long-Term Insomnia: Why Sleep Matters More Than You Think

While an occasional sleepless night might leave you feeling groggy the next day, chronic insomnia—defined as difficulty sleeping for three or more nights per week for at least three months—poses far more serious threats to your health. The consequences of long-term sleep deprivation extend far beyond fatigue, affecting virtually every system in your body and significantly impacting your quality of life.
Physical Health Consequences
Chronic insomnia takes a devastating toll on your body’s ability to function and repair itself.
Cardiovascular Disease
Long-term sleep deprivation significantly increases your risk of heart disease, high blood pressure, and stroke. During sleep, your heart rate and blood pressure naturally decrease, giving your cardiovascular system time to rest and recover. Without adequate sleep, your heart works harder, and chronic inflammation increases, leading to arterial damage and increased risk of heart attacks.
Diabetes and Metabolic Disorders
Chronic insomnia disrupts your body’s ability to regulate blood sugar levels. Sleep deprivation affects insulin sensitivity, making it harder for your cells to use glucose effectively. This can lead to type 2 diabetes, weight gain, and metabolic syndrome. Studies show that people who sleep less than 6 hours per night have a 30% higher risk of developing diabetes.
Weakened Immune System
Sleep is crucial for immune function. During deep sleep, your body produces infection-fighting cells and antibodies. Chronic sleep deprivation weakens your immune system, making you more susceptible to infections, slower to recover from illness, and less responsive to vaccines. You may find yourself getting sick more frequently and taking longer to heal.
Premature Aging and Cellular Damage
Sleep is when your body repairs cellular damage and produces growth hormone. Chronic insomnia accelerates the aging process, leading to premature wrinkles, poor skin health, and faster cellular deterioration. The lack of restorative sleep also affects your body’s ability to repair DNA damage, potentially increasing cancer risk.
Mental Health and Cognitive Impact
The brain suffers significantly from chronic sleep deprivation, affecting both mental health and cognitive function.
Depression and Anxiety
There’s a bidirectional relationship between insomnia and mental health disorders. Chronic sleep deprivation increases the risk of developing depression by 40% and anxiety disorders by 20%. Sleep helps regulate neurotransmitters like serotonin and dopamine, which are crucial for mood stability. Without adequate sleep, emotional regulation becomes increasingly difficult.
Memory and Learning Impairment
Sleep plays a vital role in memory consolidation—the process of transferring information from short-term to long-term memory. Chronic insomnia impairs your ability to form new memories, recall information, and learn new skills. This can significantly impact work performance, academic achievement, and daily functioning.
Reduced Concentration and Decision-Making
Sleep deprivation severely affects your prefrontal cortex, the brain region responsible for executive functions like attention, decision-making, and problem-solving. Chronic insomnia leads to decreased concentration, poor judgment, increased impulsivity, and difficulty processing complex information.
Increased Risk of Neurodegenerative Diseases
Emerging research suggests that chronic sleep deprivation may increase the risk of developing Alzheimer’s disease and other forms of dementia. During sleep, the brain clears out toxic proteins, including amyloid-beta plaques associated with Alzheimer’s. Without adequate sleep, these harmful proteins accumulate, potentially accelerating cognitive decline.
Safety and Performance Risks
Chronic insomnia poses immediate dangers to both personal safety and daily performance.
Increased Accident Risk
Sleep deprivation significantly impairs reaction time, attention, and decision-making abilities. Drowsy driving causes thousands of accidents annually, with sleep-deprived drivers being as dangerous as drunk drivers. The risk extends beyond driving to workplace accidents, falls, and other safety incidents that can result in serious injury or death.
Impaired Work Performance
Chronic insomnia severely impacts professional performance, leading to decreased productivity, increased errors, poor communication, and difficulty meeting deadlines. This can result in job loss, career stagnation, and financial stress, creating a vicious cycle that further exacerbates sleep problems.
The Cascade Effect
The dangers of long-term insomnia are real, serious, and far-reaching. What might seem like “just a sleep problem” can cascade into life-threatening health conditions, impaired cognitive function, and significantly reduced quality of life.
Key Takeaway
If you’re experiencing chronic insomnia, it’s crucial to seek professional help. Sleep disorders are medical conditions that require proper diagnosis and treatment. Don’t let pride or the misconception that you can “tough it out” prevent you from getting the help you need. Your health, safety, and quality of life depend on getting adequate, restorative sleep.
Understanding the Roots of Insomnia: Common Causes and Triggers
What is Insomnia: Understanding Sleep Disorders and Their Impact

Insomnia is one of the most common sleep disorders, affecting millions of people worldwide and significantly impacting their quality of life, health, and daily functioning. Far more than just occasional sleepless nights, insomnia is a complex condition characterized by persistent difficulty falling asleep, staying asleep, or achieving restorative sleep despite having adequate opportunity for rest. Understanding what insomnia truly is—its various forms, underlying causes, and wide-ranging effects—is the first step toward recognizing when sleep difficulties require attention and intervention. This comprehensive guide explores the multifaceted nature of insomnia, helping you distinguish between normal sleep variations and problematic patterns that may benefit from professional care.
Defining Insomnia: More Than Just Sleeplessness
Insomnia is a sleep disorder characterized by persistent difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate time and opportunity for sleep.
Clinical Definition and Criteria
According to medical standards, insomnia is diagnosed when sleep difficulties:
- Occur at least 3 nights per week for a minimum of 3 months (chronic insomnia)
- Cause significant distress or impairment in social, occupational, or other important areas of functioning
- Happen despite adequate opportunity for sleep (sufficient time in bed, appropriate sleep environment)
- Are not better explained by another sleep disorder, medical condition, or substance use
The key distinction is that insomnia isn’t just about the amount of sleep you get—it’s about the quality of sleep and how it affects your daytime functioning. Some people function well on 6 hours of sleep, while others need 9 hours to feel rested.
Core Symptoms of Insomnia
Nighttime Symptoms:
- Sleep Onset Difficulty: Taking more than 30 minutes to fall asleep regularly
- Sleep Maintenance Problems: Frequent awakenings during the night with difficulty returning to sleep
- Early Morning Awakening: Waking up much earlier than desired and being unable to fall back asleep
- Non-Restorative Sleep: Feeling unrefreshed despite spending adequate time in bed
Daytime Consequences:
- Fatigue, tiredness, or low energy
- Difficulty concentrating or remembering
- Mood disturbances (irritability, anxiety, depression)
- Reduced performance at work or school
- Increased errors or accidents
- Concerns or worries about sleep
What Insomnia Is NOT
It’s important to distinguish insomnia from normal sleep variations:
- Occasional sleepless nights due to stress, excitement, or environmental factors
- Short sleep duration by choice (staying up late for work or entertainment)
- Sleep disruption due to external factors like noise, light, or temperature
- Temporary sleep changes during illness, travel, or major life events
- Natural age-related changes in sleep patterns that don’t cause distress
- Sleep restriction due to work schedules or caregiving responsibilities
The key difference is persistence, impact on daily life, and the presence of adequate sleep opportunity.
Types and Classifications of Insomnia
Insomnia can be classified in several ways, helping healthcare providers understand the specific nature of sleep difficulties and develop targeted treatment approaches.
Duration-Based Classification
Acute (Short-term) Insomnia:
- Duration: Less than 3 months, often lasting days to weeks
- Triggers: Usually linked to identifiable stressors or life events
- Examples: Job loss, relationship problems, illness, travel, major life changes
- Prognosis: Often resolves on its own once the trigger is addressed
- Risk: Can develop into chronic insomnia if not properly managed
Chronic (Long-term) Insomnia:
- Duration: 3 months or longer, occurring at least 3 nights per week
- Complexity: Often involves multiple contributing factors
- Impact: Significant effects on health, mood, and quality of life
- Treatment: Usually requires professional intervention
- Patterns: May have periods of improvement and worsening
Pattern-Based Classification
Sleep Onset Insomnia (Initial Insomnia):
- Difficulty falling asleep at bedtime
- Often associated with anxiety, racing thoughts, or hyperarousal
- May involve lying awake for hours before sleep
- Common in younger adults and those with anxiety disorders
Sleep Maintenance Insomnia (Middle Insomnia):
- Frequent awakenings during the night
- Difficulty returning to sleep after awakening
- May be related to medical conditions, medications, or environmental factors
- Often seen in middle-aged and older adults
Early Morning Awakening (Terminal Insomnia):
- Waking up much earlier than desired (typically 2-4 AM)
- Unable to return to sleep
- Often associated with depression or anxiety
- May be related to circadian rhythm changes
Mixed Insomnia:
- Combination of multiple sleep difficulties
- Most complex and challenging to treat
- Often seen in chronic insomnia cases
- May require comprehensive treatment approaches
Cause-Based Classification
Primary Insomnia:
- Not directly caused by another medical or psychiatric condition
- May be related to learned behaviors or conditioned responses
- Often involves heightened arousal or sleep anxiety
- Responds well to behavioral treatments
Secondary (Comorbid) Insomnia:
- Associated with another medical, psychiatric, or substance use condition
- Examples include depression, anxiety, chronic pain, sleep apnea
- May require treatment of the underlying condition
- Can persist even after the primary condition is treated
Idiopathic Insomnia:
- Rare form beginning in childhood
- No identifiable cause or trigger
- Persistent throughout life
- May have genetic or developmental components
Common Causes and Risk Factors
Insomnia rarely has a single cause. Instead, it typically results from a complex interaction of biological, psychological, and environmental factors.
Psychological and Emotional Factors
Mental Health Conditions:
- Anxiety Disorders: Worry, racing thoughts, and physical tension interfere with sleep
- Depression: Can cause early morning awakening or difficulty falling asleep
- PTSD: Nightmares, hypervigilance, and trauma-related arousal disrupt sleep
- Bipolar Disorder: Mood episodes can significantly affect sleep patterns
Stress and Life Events:
- Work-related stress or job changes
- Relationship problems or family conflicts
- Financial difficulties
- Major life transitions (marriage, divorce, moving, retirement)
- Grief and loss
- Academic pressures
Cognitive Factors:
- Catastrophic thinking about sleep loss
- Unrealistic expectations about sleep needs
- Excessive worry about daytime consequences
- Perfectionist tendencies
Medical and Physical Factors
Medical Conditions:
- Chronic Pain: Arthritis, fibromyalgia, back pain, headaches
- Respiratory Issues: Asthma, COPD, sleep apnea
- Gastrointestinal Problems: GERD, irritable bowel syndrome
- Neurological Conditions: Parkinson’s disease, Alzheimer’s, restless leg syndrome
- Hormonal Changes: Menopause, thyroid disorders, pregnancy
- Cardiovascular Disease: Heart failure, arrhythmias
Medications and Substances:
- Stimulating Medications: Antidepressants, corticosteroids, bronchodilators
- Caffeine: Coffee, tea, energy drinks, chocolate
- Alcohol: Disrupts sleep architecture and causes fragmented sleep
- Nicotine: Stimulant effects and withdrawal symptoms
- Recreational Drugs: Various substances can disrupt sleep patterns
Environmental and Lifestyle Factors
Sleep Environment:
- Noise pollution (traffic, neighbors, snoring partners)
- Light exposure (street lights, electronic devices)
- Temperature extremes (too hot or too cold)
- Uncomfortable bedding or mattress
- Bedroom used for non-sleep activities
Lifestyle Habits:
- Irregular sleep schedules
- Excessive daytime napping
- Late-night screen time
- Large meals or fluids before bedtime
- Lack of regular exercise or exercising too close to bedtime
- Shift work or frequent travel across time zones
Age-Related Factors:
- Natural changes in sleep architecture with aging
- Increased prevalence of medical conditions
- Medication use increases with age
- Changes in circadian rhythms
- Social and lifestyle changes in older adults
Risk Factors for Developing Insomnia
Demographic Factors:
- Gender: Women are twice as likely to experience insomnia
- Age: Risk increases with age, especially after 60
- Socioeconomic Status: Lower income associated with higher risk
Personal Characteristics:
- High stress reactivity
- Tendency toward anxiety or depression
- Perfectionist personality traits
- High cognitive arousal or “racing mind”
- Family history of sleep disorders
Occupational Factors:
- Shift work or irregular schedules
- High-stress occupations
- Jobs requiring frequent travel
- Healthcare workers and first responders
The Impact of Insomnia on Health and Daily Life
Chronic insomnia extends far beyond nighttime discomfort, affecting virtually every aspect of physical health, mental well-being, and daily functioning.
Physical Health Consequences
Immune System Effects:
- Increased susceptibility to infections and illnesses
- Slower recovery from illness or injury
- Reduced vaccine effectiveness
- Increased inflammation markers in the body
Cardiovascular Impact:
- Increased risk of hypertension (high blood pressure)
- Higher risk of heart disease and stroke
- Irregular heart rhythms
- Increased stress on the cardiovascular system
Metabolic Consequences:
- Increased risk of type 2 diabetes
- Weight gain and obesity
- Disrupted hormone regulation (cortisol, growth hormone, leptin, ghrelin)
- Insulin resistance and glucose intolerance
Other Physical Effects:
- Chronic fatigue and low energy
- Headaches and muscle tension
- Gastrointestinal problems
- Premature aging and skin problems
- Reduced physical performance and endurance
Mental Health and Cognitive Effects
Mood Disorders:
- Depression: Insomnia increases risk by 2-3 times
- Anxiety: Both a cause and consequence of sleep problems
- Irritability: Increased emotional reactivity and mood swings
- Emotional Regulation: Difficulty managing stress and emotions
Cognitive Impairment:
- Attention and Concentration: Difficulty focusing on tasks
- Memory Problems: Impaired formation and recall of memories
- Decision Making: Poor judgment and increased risk-taking
- Processing Speed: Slower mental processing and reaction times
- Executive Function: Problems with planning and organization
Psychological Well-being:
- Reduced quality of life and life satisfaction
- Increased stress and worry about sleep
- Loss of confidence and self-esteem
- Social withdrawal and isolation
Impact on Daily Functioning
Work and Academic Performance:
- Decreased productivity and efficiency
- Increased absenteeism and sick days
- Higher rates of workplace accidents and errors
- Difficulty learning new skills or information
- Reduced creativity and problem-solving abilities
- Career advancement challenges
Relationships and Social Life:
- Increased irritability affecting family relationships
- Reduced social engagement and activities
- Strain on romantic partnerships
- Difficulty maintaining friendships
- Reduced empathy and social skills
Safety Concerns:
- Increased risk of motor vehicle accidents
- Higher likelihood of falls and injuries
- Workplace safety incidents
- Impaired judgment in dangerous situations
Economic Impact
Personal Financial Costs:
- Increased healthcare expenses
- Lost wages due to reduced productivity or sick days
- Costs of sleep aids and treatments
- Higher insurance premiums due to health complications
Societal Costs:
- Billions in lost productivity annually
- Increased healthcare system burden
- Costs related to accidents and safety incidents
- Disability and workers’ compensation claims
The Sleep-Wake Cycle and How Insomnia Disrupts It
Understanding normal sleep processes helps explain how insomnia develops and why it can be so disruptive to overall health and functioning.
Normal Sleep Architecture
Sleep Stages:
- Stage 1 (Light Sleep): Transition from wakefulness to sleep, easily awakened
- Stage 2 (Light Sleep): Deeper than Stage 1, brain waves slow down, body temperature drops
- Stage 3 (Deep Sleep): Slow-wave sleep, crucial for physical restoration and memory consolidation
- REM Sleep: Rapid eye movement sleep, important for emotional processing and memory
Sleep Cycles:
- Complete sleep cycles last approximately 90-120 minutes
- Healthy adults typically experience 4-6 cycles per night
- Deep sleep is more prominent in early cycles
- REM sleep increases toward morning
Circadian Rhythm Regulation
The Body’s Internal Clock:
- Located in the suprachiasmatic nucleus of the brain
- Responds to light and darkness cues
- Regulates sleep-wake cycles, body temperature, and hormone release
- Naturally runs on approximately a 24-hour cycle
Key Hormones:
- Melatonin: Promotes sleepiness, released in darkness
- Cortisol: Promotes alertness, peaks in the morning
- Growth Hormone: Released during deep sleep for physical restoration
- Adenosine: Builds up during wakefulness, creates sleep pressure
How Insomnia Disrupts Sleep
Hyperarousal Theory:
- Chronic state of heightened alertness
- Elevated stress hormones (cortisol, adrenaline)
- Increased brain activity and metabolism
- Difficulty transitioning from wake to sleep state
Conditioned Insomnia:
- Bedroom becomes associated with wakefulness and frustration
- Anxiety about sleep creates a self-perpetuating cycle
- Learned behaviors that interfere with sleep
- Cognitive arousal and racing thoughts at bedtime
Sleep Architecture Changes:
- Reduced deep sleep and REM sleep
- Increased light sleep and awakenings
- Fragmented sleep cycles
- Altered timing of sleep stages
Recognizing When to Seek Help
While occasional sleep difficulties are normal, certain signs indicate that professional evaluation and treatment may be beneficial.
Warning Signs and Red Flags
Duration and Frequency Indicators:
- Sleep problems persist for more than 2-3 weeks
- Insomnia occurs 3 or more nights per week
- Sleep difficulties are worsening over time
- Multiple self-help strategies have failed
Functional Impairment Signs:
- Significant daytime fatigue affecting daily activities
- Difficulty concentrating at work or school
- Mood changes or increased irritability
- Relationship problems related to sleep issues
- Safety concerns (drowsy driving, workplace accidents)
Physical and Mental Health Concerns:
- Development of anxiety or depression symptoms
- Increased frequency of illness
- Worsening of existing medical conditions
- Reliance on alcohol or substances to sleep
- Thoughts of self-harm or hopelessness
Self-Assessment Questions
Consider seeking professional help if you answer “yes” to several of these questions:
- Do you regularly take more than 30 minutes to fall asleep?
- Do you wake up frequently during the night and have trouble getting back to sleep?
- Do you wake up much earlier than you want to and can’t return to sleep?
- Do you feel tired and unrefreshed even after a full night in bed?
- Are you worried or anxious about your sleep?
- Is your sleep problem affecting your mood, energy, or relationships?
- Are you having trouble concentrating or remembering things?
- Have you been using sleep aids (prescription or over-the-counter) regularly?
- Are you avoiding social activities because of fatigue?
- Have others commented on your mood or performance changes?
Types of Professional Help Available
Primary Care Physicians:
- Initial evaluation and basic treatment
- Rule out medical causes
- Medication management
- Referrals to specialists
Sleep Medicine Specialists:
- Comprehensive sleep disorder evaluation
- Sleep studies and diagnostic testing
- Treatment of complex sleep disorders
- Advanced therapeutic interventions
Mental Health Professionals:
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
- Treatment of underlying anxiety or depression
- Stress management and coping strategies
- Behavioral sleep interventions
Understanding Insomnia: Your First Step Toward Better Sleep
Insomnia is a complex sleep disorder that goes far beyond simple sleeplessness. It’s a condition that can significantly impact every aspect of your life—from your physical health and mental well-being to your relationships and professional performance. Understanding what insomnia truly is, recognizing its various forms, and appreciating its wide-ranging effects is crucial for anyone experiencing persistent sleep difficulties.
Key takeaways: Insomnia is defined not just by how much sleep you get, but by how sleep problems affect your daytime functioning. It can manifest as difficulty falling asleep, staying asleep, or achieving restorative sleep, and it often involves a complex interplay of biological, psychological, and environmental factors.
Remember: Occasional sleepless nights are normal, but persistent sleep difficulties that interfere with your daily life warrant attention. Chronic insomnia can have serious consequences for your health and quality of life, but it’s also highly treatable with the right approach.
Take action: If you recognize signs of insomnia in your own sleep patterns, don’t wait for the problem to resolve on its own. Early intervention often leads to better outcomes and can prevent acute insomnia from becoming a chronic condition.
Hope for better sleep: Understanding insomnia is the first step toward overcoming it. With proper knowledge, appropriate treatment, and patience with the process, most people with insomnia can achieve significant improvement in their sleep quality and overall well-being.
Quality sleep is not a luxury—it’s a fundamental requirement for optimal health and functioning. By understanding what insomnia is and how it affects you, you’re already on the path toward reclaiming the restorative sleep you need and deserve.
Professional Treatment for Insomnia: When to Seek Help and What to Expect

While many sleep issues can be resolved with lifestyle changes and self-help strategies, chronic insomnia often requires professional intervention to break the cycle of sleeplessness. Professional treatment for insomnia has evolved significantly, offering evidence-based approaches that address both the symptoms and underlying causes of sleep disorders. From cognitive behavioral therapy specifically designed for insomnia to carefully managed medication protocols, healthcare providers now have a comprehensive toolkit to help restore healthy sleep patterns. This guide explores when to seek professional help, what treatment options are available, and how to navigate the journey toward better sleep with expert guidance.
When to Seek Professional Help
Recognizing when insomnia requires professional intervention is crucial for preventing the condition from becoming chronic and impacting your overall health and quality of life.
Signs You Need Professional Treatment
Duration and Frequency:
- Sleep difficulties persist for more than 3 months despite self-help efforts
- Insomnia occurs 3 or more nights per week consistently
- Sleep problems are getting worse rather than improving
- You’ve tried multiple self-help strategies without success
Impact on Daily Life:
- Significant daytime fatigue affecting work or school performance
- Mood changes including irritability, anxiety, or depression
- Difficulty concentrating or making decisions
- Increased accidents or near-misses due to sleepiness
- Relationship problems related to sleep issues
- Physical symptoms like headaches or digestive issues
Red Flag Symptoms
Certain symptoms warrant immediate professional attention:
- Sleep Apnea Signs: Loud snoring, gasping during sleep, morning headaches
- Restless Leg Syndrome: Uncomfortable sensations in legs with urge to move
- Parasomnias: Sleepwalking, night terrors, or violent movements during sleep
- Narcolepsy Symptoms: Sudden sleep attacks during the day
- Mental Health Concerns: Thoughts of self-harm or severe depression
- Substance Use: Relying on alcohol or drugs to sleep
Types of Healthcare Providers
Primary Care Physician:
- Often the first point of contact for sleep concerns
- Can rule out medical causes and provide initial treatment
- May prescribe short-term sleep medications
- Can refer to specialists when needed
Sleep Medicine Specialist:
- Board-certified in sleep disorders
- Specializes in comprehensive sleep evaluations
- Can diagnose complex sleep disorders
- Provides advanced treatment options
Psychologist/Therapist:
- Specializes in cognitive behavioral therapy for insomnia (CBT-I)
- Addresses psychological factors affecting sleep
- Provides non-medication treatment approaches
- Helps with stress and anxiety management
Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is considered the gold standard treatment for chronic insomnia, with research showing it’s as effective as medication in the short term and more effective in the long term.
What is CBT-I?
Cognitive Behavioral Therapy for Insomnia is a structured program that helps you identify and replace thoughts and behaviors that cause or worsen sleep problems with habits that promote sound sleep.
Core Components:
- Sleep Education: Learning about normal sleep patterns and sleep hygiene
- Cognitive Therapy: Identifying and changing negative thoughts about sleep
- Behavioral Interventions: Changing behaviors that interfere with sleep
- Sleep Restriction: Limiting time in bed to improve sleep efficiency
- Stimulus Control: Strengthening the association between bed and sleep
- Relaxation Training: Learning techniques to reduce physical and mental arousal
CBT-I Techniques in Detail
Sleep Restriction Therapy:
- Limits time in bed to match actual sleep time
- Gradually increases sleep window as sleep efficiency improves
- Helps consolidate sleep and reduce time spent awake in bed
- Typically shows results within 2-4 weeks
Stimulus Control Instructions:
- Go to bed only when sleepy
- Use bed only for sleep and intimacy
- Get out of bed if unable to sleep within 15-20 minutes
- Return to bed only when sleepy again
- Maintain consistent wake time regardless of sleep quality
Cognitive Restructuring:
- Identifies catastrophic thoughts about sleep loss
- Challenges unrealistic expectations about sleep
- Develops more balanced, realistic thoughts about sleep
- Reduces anxiety and worry about sleep
CBT-I Treatment Process
Typical Treatment Structure:
- Duration: Usually 6-8 sessions over 6-10 weeks
- Format: Individual or group sessions, in-person or online
- Homework: Sleep diaries, practice exercises, behavioral changes
- Follow-up: Booster sessions to maintain progress
What to Expect:
- Initial Assessment: Comprehensive sleep history and evaluation
- Sleep Diary: Detailed tracking of sleep patterns for 1-2 weeks
- Personalized Plan: Tailored interventions based on your specific issues
- Gradual Implementation: Step-by-step introduction of techniques
- Progress Monitoring: Regular assessment and plan adjustments
Effectiveness and Benefits of CBT-I
Research-Proven Results:
- 70-80% of people experience significant improvement
- Reduces time to fall asleep by an average of 30-50%
- Decreases nighttime awakenings
- Improves sleep quality and daytime functioning
- Benefits typically maintained long-term
Advantages Over Medication:
- No side effects or dependency risks
- Addresses underlying causes, not just symptoms
- Provides lasting skills for managing sleep
- Can be combined with other treatments
- Improves overall sleep confidence and quality of life
Medical Treatments and Medications
While CBT-I is the preferred first-line treatment, medications may be appropriate in certain situations, either as a short-term solution or in combination with behavioral therapy.
When Medication May Be Considered
Appropriate Situations:
- Severe insomnia causing significant impairment
- Crisis situations requiring immediate relief
- CBT-I is not available or accessible
- Patient preference after discussing risks and benefits
- Combination therapy with CBT-I for severe cases
- Underlying medical conditions contributing to insomnia
Goals of Medication Treatment:
- Provide short-term relief while implementing behavioral changes
- Break the cycle of chronic insomnia
- Improve daytime functioning
- Reduce anxiety about sleep
Types of Sleep Medications
Prescription Sleep Aids:
- Z-drugs (Zolpidem, Eszopiclone, Zaleplon):
- Shorter half-life than traditional benzodiazepines
- Less risk of next-day drowsiness
- Still carry dependency and tolerance risks
- May cause complex sleep behaviors
- Benzodiazepines (Temazepam, Lorazepam):
- Effective for sleep initiation and maintenance
- Higher risk of dependency and tolerance
- Can cause daytime sedation and cognitive impairment
- Generally reserved for short-term use
- Orexin Receptor Antagonists (Suvorexant, Lemborexant):
- Newer class targeting wake-promoting systems
- May have lower dependency risk
- Can cause next-day drowsiness
- Expensive and may not be covered by insurance
Off-Label Medications
Antidepressants:
- Trazodone: Commonly prescribed off-label for insomnia
- Mirtazapine: Sedating antidepressant, useful for depression with insomnia
- Doxepin: Low-dose formulation specifically for sleep maintenance
- May be preferred for patients with comorbid depression or anxiety
Antihistamines:
- Diphenhydramine (Benadryl): Available over-the-counter
- Doxylamine: Found in many OTC sleep aids
- Can cause next-day drowsiness and cognitive impairment
- Tolerance develops quickly
- Not recommended for long-term use
Other Options:
- Melatonin: Natural hormone, useful for circadian rhythm disorders
- Ramelteon: Melatonin receptor agonist
- Gabapentin: May help with sleep in certain conditions
Medication Considerations and Risks
Potential Side Effects:
- Next-day drowsiness and cognitive impairment
- Memory problems and confusion
- Increased fall risk, especially in older adults
- Complex sleep behaviors (sleep-driving, sleep-eating)
- Rebound insomnia when discontinuing
Long-term Risks:
- Physical and psychological dependence
- Tolerance requiring higher doses
- Withdrawal symptoms
- Masking underlying sleep disorders
- Potential cognitive decline with long-term use
Safe Use Guidelines:
- Use lowest effective dose for shortest duration
- Regular monitoring by healthcare provider
- Avoid alcohol and other sedating substances
- Plan for gradual discontinuation
- Combine with behavioral therapy when possible
Comprehensive Sleep Evaluation
A thorough professional evaluation is essential for identifying the underlying causes of insomnia and developing an effective treatment plan.
Initial Assessment Process
Medical History:
- Detailed sleep history including onset, duration, and patterns
- Current medications and supplements
- Medical conditions that may affect sleep
- Family history of sleep disorders
- Substance use history
Sleep Diary Analysis:
- Bedtime and wake time patterns
- Sleep latency (time to fall asleep)
- Number and duration of nighttime awakenings
- Total sleep time and sleep efficiency
- Daytime napping and caffeine intake
- Mood and energy levels
Physical Examination:
- Assessment of airway and breathing
- Neurological examination
- Evaluation for signs of other medical conditions
- BMI and neck circumference measurement
Diagnostic Tools and Tests
Sleep Study (Polysomnography):
- Comprehensive overnight monitoring in a sleep lab
- Measures brain waves, eye movements, muscle activity
- Monitors breathing, heart rate, and oxygen levels
- Can diagnose sleep apnea, periodic limb movements, and other disorders
- Usually not needed for straightforward insomnia cases
Home Sleep Testing:
- Simplified monitoring for suspected sleep apnea
- More convenient and cost-effective than lab studies
- Limited to breathing and oxygen monitoring
- May miss some sleep disorders
Actigraphy:
- Wrist-worn device that monitors movement and light exposure
- Provides objective data on sleep-wake patterns
- Useful for assessing circadian rhythm disorders
- Can be worn for weeks to capture patterns
Questionnaires and Assessment Tools
Standardized Sleep Questionnaires:
- Insomnia Severity Index (ISI): Measures insomnia severity and impact
- Pittsburgh Sleep Quality Index (PSQI): Assesses overall sleep quality
- Epworth Sleepiness Scale: Evaluates daytime sleepiness
- Sleep Hygiene Index: Assesses sleep-related behaviors
Mental Health Screening:
- Depression and anxiety assessments
- Stress and trauma history
- Cognitive function evaluation
- Quality of life measures
Specialized Treatment Approaches
Beyond CBT-I and medication, several specialized treatments may be recommended for specific types of insomnia or when standard approaches aren’t sufficient.
Light Therapy
Particularly effective for circadian rhythm disorders and seasonal sleep issues.
How It Works:
- Uses bright light to reset the body’s internal clock
- Suppresses melatonin production at appropriate times
- Helps synchronize circadian rhythms
- Can advance or delay sleep timing as needed
Treatment Protocol:
- Typically uses 10,000 lux light boxes
- Treatment duration: 30 minutes to 2 hours daily
- Timing depends on desired circadian shift
- Morning light advances sleep phase (earlier bedtime)
- Evening light delays sleep phase (later bedtime)
Conditions Treated:
- Delayed Sleep Phase Syndrome
- Advanced Sleep Phase Syndrome
- Shift Work Sleep Disorder
- Jet Lag
- Seasonal Affective Disorder
Mindfulness-Based Interventions
Combines meditation and mindfulness practices with sleep-specific techniques.
Mindfulness-Based Stress Reduction (MBSR):
- 8-week program focusing on stress reduction
- Includes body scan meditation and mindful breathing
- Helps reduce anxiety and racing thoughts
- Improves overall stress management
Mindfulness-Based Therapy for Insomnia (MBTI):
- Specifically designed for sleep problems
- Combines mindfulness with sleep education
- Focuses on accepting and observing sleep difficulties
- Reduces sleep-related anxiety and effort
Benefits:
- Reduces pre-sleep arousal and worry
- Improves emotional regulation
- Enhances overall well-being
- Can be combined with other treatments
Biofeedback and Relaxation Training
Teaches conscious control over physiological processes that affect sleep.
Types of Biofeedback:
- EMG Biofeedback: Monitors muscle tension
- EEG Biofeedback: Monitors brain wave activity
- Heart Rate Variability: Monitors autonomic nervous system
- Temperature Biofeedback: Monitors peripheral blood flow
Progressive Muscle Relaxation:
- Systematic tensing and relaxing of muscle groups
- Reduces physical tension and anxiety
- Can be learned and practiced independently
- Particularly helpful for stress-related insomnia
Sleep Restriction and Consolidation
Advanced behavioral techniques for severe insomnia cases.
Intensive Sleep Restriction:
- More aggressive limitation of time in bed
- May initially restrict sleep to 4-5 hours
- Requires close professional monitoring
- Can produce rapid improvements in severe cases
Sleep Consolidation Therapy:
- Focuses on creating continuous, uninterrupted sleep
- May involve temporary sleep deprivation
- Rebuilds natural sleep drive
- Typically done in controlled clinical settings
Treatment for Comorbid Conditions
Insomnia often occurs alongside other medical or psychiatric conditions, requiring integrated treatment approaches.
Insomnia and Mental Health
Depression and Insomnia:
- Bidirectional relationship – each condition can worsen the other
- May require treatment of both conditions simultaneously
- Antidepressants may improve or worsen sleep
- CBT-I can be effective even with comorbid depression
Anxiety Disorders:
- Racing thoughts and worry interfere with sleep onset
- May benefit from anxiety-specific CBT techniques
- Relaxation training particularly helpful
- Some anxiety medications can affect sleep
PTSD and Trauma:
- Nightmares and hypervigilance disrupt sleep
- May require trauma-specific therapy
- Image Rehearsal Therapy for nightmares
- EMDR may help with trauma-related sleep issues
Medical Conditions and Sleep
Chronic Pain:
- Pain interferes with sleep initiation and maintenance
- Poor sleep can increase pain sensitivity
- May require coordinated pain and sleep management
- Sleep positioning and comfort measures important
Hormonal Changes:
- Menopause-related sleep disruption
- Thyroid disorders affecting sleep
- Hormone replacement therapy considerations
- Age-related changes in sleep architecture
Neurological Conditions:
- Parkinson’s disease and sleep disorders
- Alzheimer’s disease and circadian disruption
- Multiple sclerosis and fatigue
- Epilepsy and sleep-seizure interactions
Integrated Treatment Approaches
Multidisciplinary Care:
- Coordination between sleep specialists, psychiatrists, and primary care
- Shared treatment goals and communication
- Regular monitoring and plan adjustments
- Patient education about condition interactions
Medication Considerations:
- Review all medications for sleep effects
- Timing of medications to minimize sleep disruption
- Drug interactions and contraindications
- Gradual changes to avoid withdrawal effects
Finding the Right Treatment Provider
Choosing the right healthcare provider is crucial for successful insomnia treatment.
Questions to Ask Potential Providers
About Their Experience:
- How many patients with insomnia do you treat?
- What is your training in sleep medicine?
- Are you board-certified in sleep medicine?
- Do you offer CBT-I or can you refer to someone who does?
About Treatment Approach:
- What is your typical approach to treating insomnia?
- Do you prefer behavioral or medication treatments?
- How do you handle treatment-resistant cases?
- What role do you see for sleep medications?
About the Process:
- What can I expect during the evaluation?
- How long does treatment typically take?
- How often will we meet?
- What homework or assignments will be involved?
Insurance and Cost Considerations
Insurance Coverage:
- Check if sleep medicine consultations are covered
- Verify coverage for CBT-I sessions
- Understand copays and deductibles
- Ask about prior authorization requirements
Alternative Options:
- Online CBT-I programs (often more affordable)
- Group therapy sessions
- Community mental health centers
- University training clinics
- Employee assistance programs
Preparing for Your First Appointment
Information to Gather:
- Complete sleep diary for 1-2 weeks
- List of all medications and supplements
- Medical history and previous sleep treatments
- Questions and concerns about your sleep
What to Expect:
- Detailed discussion of sleep history
- Physical examination if indicated
- Discussion of treatment options
- Development of initial treatment plan
- Scheduling of follow-up appointments
Your Path to Professional Sleep Care
Professional treatment for insomnia offers hope and effective solutions for those struggling with chronic sleep problems. With evidence-based approaches like CBT-I leading the way, and carefully managed medication options when appropriate, healthcare providers can help break the cycle of insomnia and restore healthy sleep patterns.
Remember: Seeking professional help is not a sign of weakness—it’s a proactive step toward better health and quality of life. Chronic insomnia can have serious consequences for your physical and mental health, relationships, and daily functioning.
Take action: If you’ve been struggling with sleep for more than a few weeks, or if insomnia is significantly impacting your life, don’t wait. Start with your primary care physician or seek out a sleep specialist or CBT-I trained therapist.
Be patient: Professional treatment takes time to work, especially behavioral approaches. Most people see significant improvement within 6-8 weeks of starting CBT-I, but some benefits may continue to develop over months.
Stay engaged: Success in professional treatment requires active participation. Be honest with your provider, complete assignments, and communicate about what’s working and what isn’t.
Quality sleep is not a luxury—it’s essential for your health and well-being. Professional treatment can help you reclaim the restorative sleep you need and deserve.
How to Deal with Insomnia: A Comprehensive Guide to Better Sleep
The Devastating Harm of Chronic Insomnia: Understanding Long-Term Consequences

Slumbelry Concierge
Sleep Deeper. Live Better.
Secure & Private. Only for our reply.